

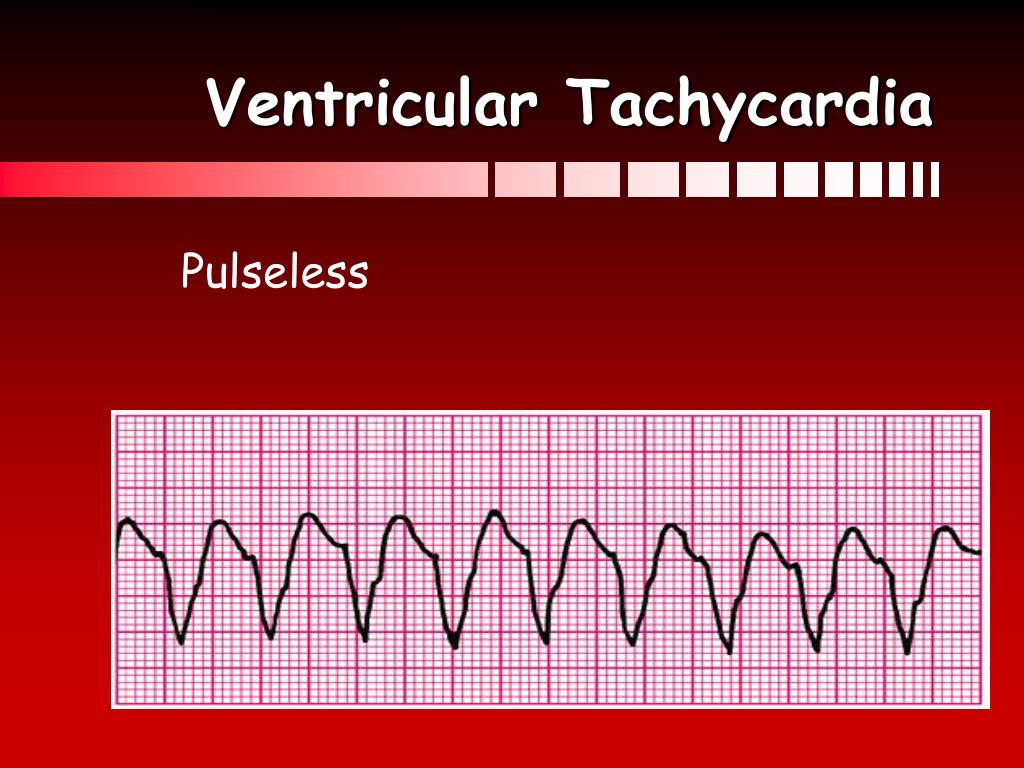
What are the causes of these altered trends? If VF were more likely to manifest among patients with coronary artery disease (CAD), the significant drop in mortality from CAD might explain the decline in VF cases. 5 Therefore, the rising prevalence of PEA has significant public health implications. There is a stark contrast between success rates for PEA (≤6%) 4 compared with VF/VT (as high as 40%). 3 Another consistent finding is that success rates of resuscitation from SCA are a function of the presenting arrhythmia. 2 Similarly, in Helsinki, Finland, the prevalence of VF decreased by 48% from 1994 to 1999. 1 In Goteborg, Sweden, the proportion of VF cases decreased from 39% in 1981 to 32% in 1997, whereas PEA cases increased from 6% to 26% in the same time period. Among residents of Seattle, Wash, aged ≥20 years, there was a 56% decrease in VF from 1980 to 2000. There has been a progressive increase in the proportion of sudden cardiac arrest (SCA) cases presenting with pulseless electrical activity (PEA), due in large part, to a decrease in the prevalence of ventricular fibrillation (VF). In a subgroup analysis of resting ECGs (n=391), there were no differences in cardiac clinical history or prevalence of cardiac conduction system disease (PEA, 31.6% versus VF, 32.2% P=0.48). Pulmonary disease and female gender were significant factors associated with PEA ( P for interaction=0.04). Black race was also independently associated with PEA (odds ratio, 2.6 confidence interval, 1.3 to 5.4). A history of syncope was strongly associated with PEA (odds ratio, 2.6 confidence interval, 1.3 to 5.3) after adjustment for age, gender, response time, and arrest circumstances. Compared with VF cases, PEA cases were older (mean age, 68 versus 63 years P=0.0002), more likely to be female (37% versus 26% P=0.0008), and less likely to survive to hospital discharge (6% versus 25% P<0.0001). Presenting arrhythmia was VF in 48%, PEA in 25%, and asystole/other in the remainder. A total of 1277 cases aged ≥18 years underwent resuscitation by first responders (mean age, 65☑6 years 67% male). Those presenting with PEA versus VF and asystole were compared with χ 2 tests, ANOVA, and logistic regression. In the Portland, Ore, metropolitan area (population ≈1 million), cases of out-of-hospital sudden cardiac arrest who underwent attempted resuscitation were identified prospectively (2002–2007). Customer Service and Ordering Information.Stroke: Vascular and Interventional Neurology.

Journal of the American Heart Association (JAHA).Circ: Cardiovascular Quality & Outcomes.

Although there is no evidence that atropine has a detrimental effect during bradycardia or asystolic cardiac arrest, routine use of atropine during PEA or asystole has not been shown to have a therapeutic benefit.


 0 kommentar(er)
0 kommentar(er)
